- July 14, 2023
- Saloni Kabra
- 0
It has been established that bipolar disorder is not brought on by a specific person, circumstance, or experience. This disorder can develop in some people as a result of a number of interconnected factors. Let’s try to comprehend how all of these elements interact to cause the development of this condition.
First, we start by examining the three main factors—genetic vulnerability, biological vulnerability, and socio-environmental stress (or life stress)—that determine how vulnerable we are to developing this condition.
- Genetic Vulnerability– Bipolar disorder is more likely to run in families due to genetic susceptibility. Compared to the general population, children of bipolar patients have an 8% greater chance of developing the illness. The risk of unipolar depression in children of bipolar patients (depression only, without mania) is also increased (12%). These findings support the genetic predisposition of this disorder to some extent, but they also raise the possibility of other risk factors.
- Biological Vulnerability: This term describes potential biochemical imbalances in the brain that predispose a person to having mood swings. Episodes of “high” or “low” moods may be brought on by an imbalance of brain chemicals such as noradrenaline, serotonin and dopamine or a failure of these chemicals to function properly.
- Socio Environmental Stress: A person may experience socio-environmental stress as a result of stressful life events or circumstances such as family conflicts, work-related challenges, bereavement, or even happy life events like getting married, having children, moving houses, etc. These events or circumstances can place additional demands on the person and cause them to feel stressed, frustrated, anxious, sad, etc.
Thus, the occurrence of bipolar disorder can be attributed to the interaction of the aforementioned factors. A person who is genetically and/or biologically vulnerable may not necessarily develop bipolar disorder. How they respond to stressors in their lives has an impact on these vulnerabilities. A person with a family history of depression, for instance, may be able to manage their vulnerability to developing the disorder if they look out for warning signs, are aware of their own vulnerabilities—genetic and environmental—and develop appropriate coping skills with a strong support structure. This brings us to a discussion on “protective and risk factors.”
PROTECTIVE & RISK FACTORS
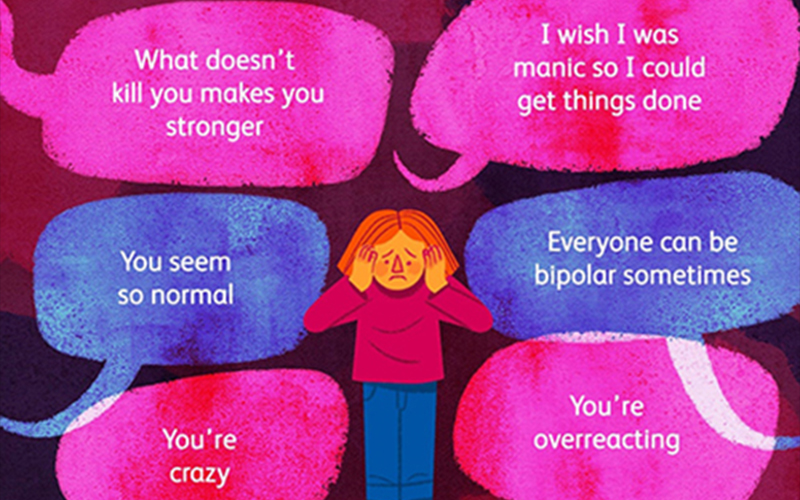
- A risk factor is something that will increase the chances of a person who is already vulnerable becoming ill. Poor or inappropriate coping mechanisms,
alcohol or drug use, irregular daily schedules, interpersonal conflicts, stressful situations, noncompliance with medication, inadequate social support,
psychosocial impairment, etc. are a few examples of risk factors.
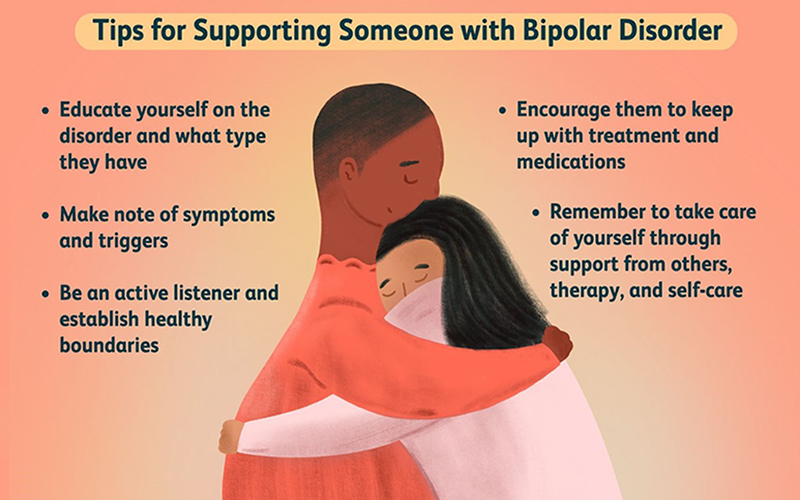
- On the other hand, protective factors work to keep a vulnerable person from getting sick. Good coping mechanisms, strong social networks, adherence to medication, a regular, balanced lifestyle, skillful communication, and others are protective factors.
The likelihood of developing the disorder is greatest when the risk factors outweigh the protective factors. This idea also holds true when taking into account the possibility of recurrence.
Let’s make a Stress-Vulnerability flowchart of our own: